I had the privilege of participating in the incredible Lake Nona Impact Forum and speaking with one of the most influential and brilliant minds in medicine: Dr. Francis Collins. Dr. Collins and I discussed highlights from his monumental career, emerging technologies that are transforming health care and the “current obsession” that is driving him into the future.
The annual Lake Nona Impact Forum focused on building the “Wellbeing Ecosystem of the Future” by exploring the intersections of health, wellness, medical and scientific innovation and strategies to optimize human performance.
Dr. Collins is a living testament that science and faith do not need to be at odds. In fact, one can inform the other to make a better world for all. We hope you can each apply some of Dr. Collins’ powerful insights to your own life and practice.
A conversation with Dr. Francis Collins
The impact and influence of physician-geneticist Dr. Francis Collins on human well-being is almost impossible to capture. As the longest- serving director of the National Institutes of Health (NIH)—spanning 12 years and three presidencies—he oversaw the work of the largest supporter of biomedical research in the world.
Before leading the NIH, Dr. Collins made numerous landmark discoveries of disease genes and spearheaded the international Human Genome Project. The project culminated in April 2003 with the completion of a finished sequence of the human DNA instruction book that is fundamentally changing how we understand human health and disease. Dr. Collins served as director of the National Human Genome Research Institute at the NIH from 1993 to 2008.
Dr. Collins’ research laboratory is currently based at the NIH. Over the last several decades, he and his team were responsible for multiple important discoveries such as genes causing cystic fibrosis, neurofibromatosis, Huntington’s disease, a familial endocrine cancer syndrome and, most recently, type 2 diabetes and Hutchinson-Gilford progeria syndrome. Each of these genetic discoveries has cracked open life-changing therapeutic opportunities for patients worldwide.
With a calm hand, an exceptional scientific mind and a visionary commitment to public service, Dr. Francis Collins has helped save thousands of people’s lives and improved the health of millions more.
In issue 14 of CuraLink, Dr. Collins shares his perspective on the most critical issues of our time and the collaborative path toward solving them.
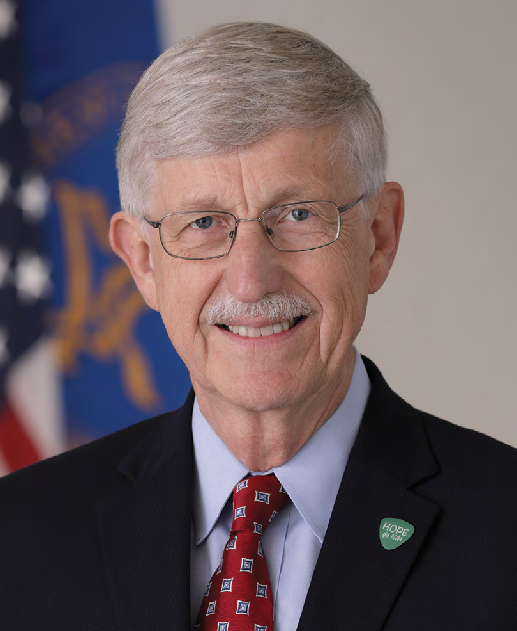
Francis Collins, MD, PhD, Special Projects Advisor to President Biden and 16th Director, National Institutes of Health
You directed the National Institutes of Health for over 12 years, previously led the Human Genome Project and conducted groundbreaking research at Yale University and the University of Michigan. What accomplishment or advancement are you most proud of?
I have had the privilege to be involved in groundbreaking biomedical research for most of my life, and many opportunities have well outstripped what I thought possible. Time and again, the best and brightest came together across disciplines: Sparks ignited, discoveries were made and many people benefited.
When I was an assistant professor at Michigan, we collaborated with a group in Toronto and discovered the cystic fibrosis (CF) gene during a long, tortuous process. It took 30 years for that discovery to lead to an effective treatment, but many people with CF, who were expecting their lives to be cut short, are now planning their retirements. The therapy that came out of that discovery had this miraculous benefit for young people with CF.
Moving forward, the Human Genome Project was an incredible opportunity for me to lead a team of 2,400 scientists in six countries, all collaborating and sharing data every 24 hours so people could start using it to produce the first instruction book for human biology. When the human genome was completed in 2003, we felt like we had crossed over a bridge into new territory. Now, we have to continue to learn about how to read it and understand it. That has been an intense effort over the last 20 years and will continue for decades to come.
Then, more recently as the NIH Director, with help from many scientific and non-scientific advocates, I had the chance to help initiate the BRAIN (Brain Research Through Advancing Innovative Neurotechnologies®) Initiative. Project scientists are trying to understand how the 86 billion neurons between your ears do what they do. How do brain circuits perform complex functions, and what happens when they don’t function properly and disease occurs? That level of understanding of the brain has been completely out of reach, but now we can see the path forward. If you really want answers to schizophrenia, Alzheimer’s disease, Parkinson’s disease and all of the mental illness issues we’re facing, you need to understand how the brain works. The science to answer those questions is progressing with remarkable speed.
And then there’s gene therapy. As a postdoc in the early 1980s, I studied sickle cell disease, an illness that mostly affects African Americans. I hoped that somehow in my lifetime we could find a cure for the first molecular disease that causes unimaginable pain. Now we have a few instances of not only ameliorating some of the dreadful symptoms but also curing the disease using CRISPR/Cas9 gene editing. The FDA is now reviewing this body of data. It’s possible that we will see an approved curative therapy this year for the ~100,000 Americans with sickle cell disease.
Lastly, we need to push these breakthroughs forward as global health advances. Over the last 15 years, I’ve tried to focus on all people needing medical research, not just those in the developed world. As an example, most people with sickle cell disease live in Sub-Saharan Africa, where having a single copy of that misspelled gene was selected for because it provides resistance to malaria. But two copies of this same mutation cause sickle cell disease and untold pain, suffering and death. Most kids with sickle cell disease in Nigeria or Cameroon don’t make it to age 5. In collaboration with the Bill & Melinda Gates Foundation, we are determined to develop a sickle cell cure that doesn’t require a tertiary care medical center. We are seeking to develop a gene therapy that can be delivered in one intravenous injection in an outpatient, low-resource setting with a 95% success rate. We hope to get there in the next decade.
Since you stepped away from your post as Science Advisor to the President, how are you spending your time? What is your lab focused on?
My lab at the NIH is working on two diseases. One is type 2 diabetes. We are teasing apart the genetic and environmental risk factors for this disease that causes extensive morbidity and mortality across the world. Our focus is on using stem cells and CRISPR/Cas9 modifications to understand those hundreds of places in the genome where a small change increases your risk of diabetes. We want to understand the mechanism behind those genetic risks and how that information can be used to implement the practice of precision health for each individual.
The second disease we’re studying is an extremely rare condition called progeria, the most dramatic form of premature aging. These kids appear normal at birth but then start aging at about seven times the normal rate, even though their intellectual development is that of a normal child. Untreated, they typically die around age 13 from heart attacks and strokes. Progeria is heartbreaking, devastating and tragic. We discovered its cause: It’s a single-letter genetic mutation in the LMNA (“lamin A”) gene, which produces a protein that helps maintain the normal structure and function of a cell’s nucleus. The mutation creates a toxic form of the protein.
The discovery of the causative mutation led us and our collaborators to develop a drug that the FDA has approved and that extends a progeria patient’s life by several years. But that’s not good enough. We want to actually fix that mutated gene and return it to its normal sequence using a base editor—like “find and replace” in your word processor, except the document is the genome. In another year or two, we hope to be running that clinical trial in humans, because the approach works remarkably well in a mouse model.
But though I’m very engaged in research on diabetes and progeria, I still have a role in the White House. In October when I stepped down as the acting Science Advisor, I was asked to stay on as Special Projects Advisor to President Biden. I am focused on an opportunity that has become my current obsession and involves distributing a cure to people in need.
Two and a half million people in the U.S. have hepatitis C, and the disease kills 15,000 people every year. It’s a virus acquired from contaminated blood—from a tattoo needle, intravenous drug use or a transfusion that was delivered before 1993 before we knew how to screen for it.
It’s a simple, highly effective oral therapy—one pill a day, for 8-12 weeks, with virtually no side effects and a 97% cure. So why aren’t people getting it? Well, it’s a reflection on our healthcare system. The cost for therapy can be up to $94,500 per patient. If you are on Medicaid, managers will say that they don’t have that in their budget and will create barriers to access. They’ll say that a patient must first have liver failure to qualify. But isn’t that what we’re trying to prevent?
Many people with hepatitis C are in marginalized communities and are not currently getting access to the cure. Without treatment, they will develop liver failure, cirrhosis and/or cancer, and may eventually need a liver transplant. The cost to our healthcare system downstream will be far greater than the cost of getting those same people cured now, especially with creative approaches to reduce the cost.
My brother-in-law died of hepatitis C. The last 3 years of his life were really grim. You wouldn’t wish that on anybody. We have to come up with a way to get the therapy to the people who need it. I believe that is not only possible, it’s essential. It’s compassionate, and it’s good healthcare economics.
What are the major lessons you learned from COVID-19?
On January 10, 2020, when the sequence of the SARS-CoV-2 virus first appeared, the NIH team of Dr. Barney Graham and Dr. Kizzmekia Corbett got to work. The design of the NIH-Moderna mRNA vaccine was basically done in about 48 hours. The very first phase of the human trial happened less than 70 days later, which is five
times faster than has ever happened in history. The scientific community kicked itself into gear with every resource possible to address the worst pandemic in 100 years. Phase 3 vaccine trials began by the end of July, enrolling 30,000 study subjects. We were especially motivated and creative in reaching out to communities who, for good reason, were skeptical about participation. Ultimately, those phase 3 trials enrolled 35-40% racial and ethnic minorities.
As a randomized controlled double- blind trial, neither the investigators nor the subjects knew who was getting a placebo or the vaccine. After a few weeks of participation, you could then measure who was getting sick and who wasn’t.
Most vaccines fail. For most vaccines that work, you’re lucky if they’re 50 or 60% effective, and most have unanticipated side effects that are common. In November, when the results were unblinded, we saw that the efficacy of both Moderna’s and Pfizer’s vaccines was 95%. The evidence of safety in the group of 30,000 people looked extremely good.

Dr. Francis Collins in conversation with Dr. Robin Smith at the Lake Nona Impact Forum. The event focused on building the “Wellbeing Ecosystem of the Future” by exploring the intersections of health, wellness, medical and scientific innovation and strategies to optimize human performance
The revelation of the trial results was such a monumental moment. At the time, people were dying all around us from COVID-19. I had dreamed, prayed and wished in every way that we would have something to offer people. Fi- nally, we had a really good vaccine we could use to end this terrible scourge. I both celebrated and had a good cry.
For a few months, it seemed like tens of millions of vaccines were going into arms, and we were going to accomplish our goal. But by the summer of 2021, it became clear that a lot of people just weren’t interested in getting vaccinated. The information they heard suggested that it didn’t work or it wasn’t safe.
Social media fueled that in a big way—as, regrettably, did some politicians. To this day, 50 million people in the U.S. continue to say COVID-19 vaccines aren’t for them. Recently, scientists did a sophisticated analysis looking at the consequences of that misinformation. They estimated that 300,000 people died in the U.S. because of misinformation about the vaccine. Three hundred thousand people who, based on what they had heard and believed to be true, opted out of getting vaccinated and then, subsequently, fell ill and died. Most of those were older people, but their lives didn’t need to end this way—and there are many other heartbreaking stories of people who died of COVID-19 in their 30s and 40s. That tragic situation made me realize that if we have a public health problem with this pandemic, it’s not just about knowing what to do. It’s about how to communicate information in a way that makes sense to people.
As one of those communicators, I have to ask myself what I could have done better. I was probably failing to emphasize early in the pandemic how uncertain we were about how this virus was going to behave. We made recommendations that were the best we had at the time, but we should have warned people that those recommendations were probably going to need revision because of incomplete data. That’s how science works.
We also didn’t do a good job of countering misinformation. Some people say we should have had a “pre- bunking” plan even before the misinformation started. We should have said: “When you start to hear this claim, you should not take it seriously. Here’s the actual evidence.”
We didn’t have a program like that, and misinformation spread much more rapidly than the truth. It contributed to the culture wars that are now inflaming our country. And of course, this is a case where culture wars didn’t just cause a lot of distress and confusion, they caused a lot of deaths. When it comes to public health, we have to figure out better ways to transmit objective information in a way that people can understand and trust.
Both you and FDA Commissioner Dr. Robert Califf have discussed how misinformation is jeopardizing public health and safety. How can public health institutions and scientific experts regain people’s trust?
Empowering a local approach is probably the most important strategy—not counting solely on high-level government sources, no matter how authoritative, because people’s trust in public institutions has deteriorated.
We should enlist the talents of people who are interested in science and are somewhat more knowledgeable than the average person—high school teachers who teach science, college students who are science majors, healthcare providers and members of scientific societies. We should create
a “science communication corps.” This corps would need to be empowered with accurate and accessible information and could blanket communities with expertise and provide people with evidence-based information.
Instead of a very top-down way of sharing information, we might get better results from a grassroots strategy. This is a big, complicated and challenging thing to do right. Now, a lot of individual groups are beginning to attempt this approach, but they’re not connected.
We should turn this scattershot approach into a consortium.

Dr. Collins is one of the most influential and brilliant minds in medicine today. He was the longest- serving director of the NIH, spearheaded the international Human Genome Project and made numerous landmark discoveries of disease genes
You’ve been very vocal about how science and faith can inform one another and don’t have to be at odds. What about science and politics?
We are in a tough spot right now, where almost everything in our country has become divisive. Politics and science are in a strange and dangerous relationship. It is assumed now that if you’re a supporter of science, then you’re more on the left side of the political spectrum. If you’re a skeptic, then you’re on the right. That’s crazy.
Then add in faith. I am a person of faith. I see no conflict between being a rigorous scientist and one who seeks answers to other questions about love, meaning, morality and beauty through the lens of faith. But I think many people of faith have been particularly vulnerable to COVID-19 information that is, frankly, not well-founded and that is often more political than scientific. The number one group of resistors to COVID-19 vaccines are white evangelical Christians. I’m also a white evangelical Christian. This breaks my heart. There are many forces that are feeding into that attack on the truth. We have to turn this around. Whether playing out in public health, the reality of climate change or the legitimacy of elections, this is a destructive circumstance for our country’s future.
March 8 was International Women’s Day, celebrating women’s achievements. You’ve always been an early champion of enhancing diversity and gender parity, especially in science and the workforce, having overseen 18,000 employees at the NIH. How are we doing when it comes to these issues?
We’re doing better than we were 15 or 20 years ago, but not well enough to be celebrating. Gender parity has been a major priority for me at the NIH. It was clear that we had a lot of women coming into biomedical research, but we were not seeing proportional levels of women getting promoted into leadership roles. For the 27 institutes at the NIH, one of my jobs as director was to hire new Institute directors. When I started, we had three women. When I left 12 years later, we had 13.
We have not done as well with encouraging other kinds of diversity. Certainly, when it comes to African Americans and Latinos/Latinas, we are still way less represented in science positions than the proportion of the American public. It’s not acceptable to say it’s just a pipeline problem, because that’s no longer true. The number of African Americans getting PhDs has been increasing steeply, but the number of African Americans in tenure-track positions in academia has been going up very slowly. There’s a mismatch there, which means we’re not doing our job to find those talented individuals and give them the opportunity to advance. To address this issue at the NIH, we started a large, bold program called UNITE. This is a broad, ambitious initiative that the NIH leadership supports, and we expect to be held accountable.
This isn’t just a nice thing to do.
“The data shows you over and over again that diversity correlates with productivity.”
If you want the most amazing, innovative science, you have to make sure you have a diverse workforce.
What are the top three emerging technologies that are poised to transform or are already transforming health care as we know it?
First: Gene editing and the CRISPR/Cas9 revolution. CRISPR/Cas9 is being widely used as a tool in human biology research labs worldwide—not just to knock out genes but to modify them, turn them down or accentuate their function.
Second: Stem cell science is another amazing breakthrough that has emerged in the last 2 decades. Mature skin or blood cells can be reprogrammed to induce a pluripotent state, where the cell is capable of differentiating into any tissue in the body if given the right signals. We may eventually be able to build entire organs from induced pluripotent stem cell lines.
Third: Gene therapies. The ability to deliver a gene to the right tissue at the right time for the 6,500 genetic diseases where we have identified the underlying DNA mutation. About 500 of these diseases currently have a treatment, the rest don’t. We need to create a streamlined, generic approach for all of these diseases.

With technology advancing at a breakneck speed and public health at the forefront, Dr. Collins believes we are in the “golden age” of medical research
Based on where the mutation is, you need a base editor to repair that mutation and a “delivery truck,” probably a virus or a nanoparticle that is programmed to go to the right tissue. Then you would have a scalable way to treat thousands of diseases without having to tackle each one in a single program that could take decades. We should be devoting all our energy into developing the base editors and delivery trucks to make this a reality. This will have an unimaginably powerful impact on rare diseases.
Artificial intelligence (AI) overlays all of this. Many future breakthroughs in biology and medicine will depend upon continuing to push machine learning and AI to the next level. In many ways, the greatest opportunities for AI are in life science. If you’re really trying to understand how the brain works, our brains may not be complicated enough to understand themselves. That’s where AI can help. You need to be careful about it, of course, especially if you’re talking about applying AI to something with clinical implications. AI is only as good as what you’ve fed it. A lot of AI training sets are biased information.
How can healthcare regulators embrace potential beneficial applications while safeguarding the public from potential harm?
You mentioned the top regulator Dr. Robert Califf who leads the Food and Drug Administration. He gets criticized every day about whether he’s been too easy or hard on something. But regulators are doing their best. We depend on them to be scientifically sophisticated and rigorous in their data analysis and to try to keep a balance of advancing innovation but also protecting against unexpected bad outcomes. Regulators have a tough job.
What are the downstream effects of these advancing technologies?
We are seeing major breakthroughs. We now have the first approved treatment for Alzheimer’s disease: a monoclonal antibody. If treated very early on, you reduce the progression by 24%. That is not yet as powerful as we hope for. But it’s a big difference from having nothing.
One question that comes along with all of these advancements is: How do we pay for all this? The Centers for Medicare & Medicaid Services has a lot on its shoulders and is working intensively in a very difficult environment. It’s estimated that the sickle cell gene therapy cure is going to cost $2-3 million per patient. You can argue that it’s still a good deal compared to the way uncured sickle cell disease will run up hospital bills. But we’re not very good at paying now to save money later, and that would be necessary in this case.
“We are in the golden age of medical research.”
We are on an exponential curve of the acquisition and application of new knowledge. The slowness of clinical application always frustrates me because I want change to happen immediately, and that takes a lot of time. But we have to do this carefully, keeping in mind that we are also committed to doing no harm.
This is an amazing time for biomedical research. Our understanding of the genome and the field of biology is taking us in directions that are transformative—both for rare and common diseases. It’s truly exciting to be part of this revolution. We want the next generation to come and join us!
This interview has been edited for length and clarity.
If you have any questions or feedback, please contact: curalink@thecurafoundation.com
Newsletter created by health and science reporter and consulting producer for the Cura Foundation, Ali Pattillo, consulting editor, Catherine Tone, and associate director at the Cura Foundation, Svetlana Izrailova.