In this CuraLink, we hear from biotech entrepreneur Dr. Noubar Afeyan. Dr. Afeyan is the co-founder and chairman of Moderna as well as the founder and chief executive officer of Flagship Pioneering.
Dr. Afeyan’s renegade entrepreneurial spirit and technical insight into the future of biotechnology offers a useful playbook to all innovators working on improving human health.
A conversation with Dr. Noubar Afeyan
From agriculture to infectious disease, Dr. Noubar Afeyan has spent over 30 years building companies to help alleviate the world’s most critical threats to human flourishing. Through his life sciences innovation company, Flagship Pioneering, Dr. Afeyan has helped launch more than 100 scientific ventures, 50 drugs in clinical development and over 500 patents, that have resulted in over $140 billion in value. Flagship’s portfolio includes the biotech and pharmaceutical company, Moderna, which developed the lifesaving mRNA-based COVID-19 vaccine.
Dr. Afeyan’s “immigrant mindset,” which fuels these broadly impactful endeavors, stems from his early experiences fleeing Lebanon during the civil war in 1975 and immigrating to Canada. This disruptive experience fostered Dr. Afeyan’s adaptability and creativity, which he later applied to his trailblazing career at the cutting edge of biotech innovation.
In issue two of CuraLink, Dr. Afeyan shares the power of the immigrant experience, the urgent need to rethink health care interventions and the five technologies that will revolutionize the next decade of medicine.
Read on to hear excerpts from Dr. Afeyan’s luminary session with Alan Murray, chief executive officer of Fortune Media, at the 2022 Lake Nona Impact Forum, as well as his conversation with Dr. Robin Smith, founder and president of the Cura Foundation.
How does your immigrant experience shape your entrepreneurial philosophy and guide your efforts to improve the human condition?
I think the immigrant experience and an immigrant mindset, whether you have the physical experience or not, help a lot. Immigrants, essentially, are innovators in that they go to a new physical space, they adapt, and they start innovations. You leave behind the comfort of your home. You have to pick up a new language. People make fun of you. You do not really belong, and you work really hard to create a new reality in which you do belong. If that reality is a totally new thing, you have innovated and you have helped the world.

Noubar Afeyan, PhD, Co-Founder & Chairman of Moderna and Founder & Chief Executive Officer of Flagship Pioneering
So, this kind of journey, that I would call surviving and then striving to thrive, is very common in what refugees go through and what innovators do, especially when they work at the cutting edge. Both mindsets are incredibly useful.
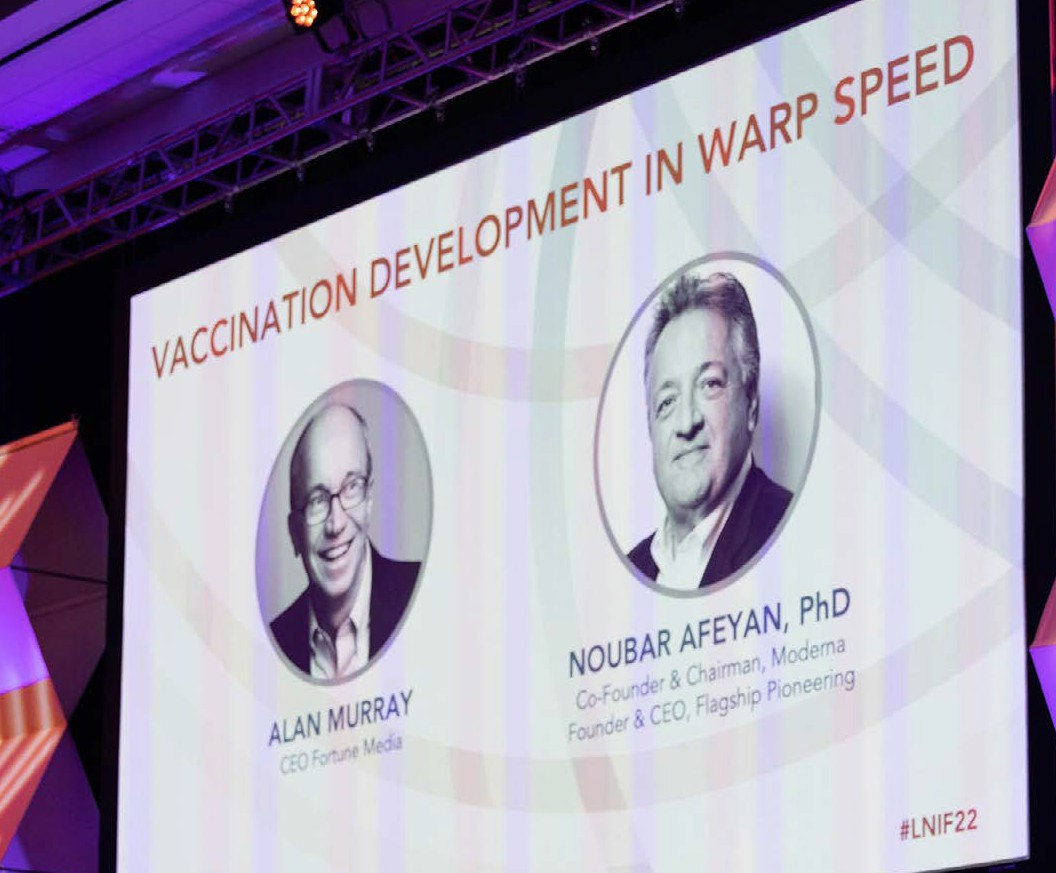

Dr. Noubar Afeyan and Alan Murray at the 2022 Lake Nona Impact Forum
How does your immigrant experience shape your entrepreneurial philosophy and guide your efforts to improve the human condition?
I think the immigrant experience and an immigrant mindset, whether you have the physical experience or not, help a lot. Immigrants, essentially, are innovators in that they go to a new physical space, they adapt, and they start innovations. You leave behind the comfort of your home. You have to pick up a new language. People make fun of you. You do not really belong, and you work really hard to create a new reality in which you do belong. If that reality is a totally new thing, you have innovated and you have helped the world.
So, this kind of journey, that I would call surviving and then striving to thrive, is very common in what refugees go through and what innovators do, especially when they work at the cutting edge. Both mindsets are incredibly useful.
Let’s talk a little more about mindsets. What does it take to crack the innovation code?
I have a little 10-dollar souvenir that I bought one day in Cape Cod. It is carved in wood and says: Trust your crazy ideas. I have had it for 20 years. ‘Trust your crazy ideas’ is an interesting formulation because trust is supposed to only be in things that are real, believable, reasonable and tested. And yet, if you trust your crazy ideas, then you will actually work on the things that you trust, such that they actually become trustworthy. So, belief and faith in what you are working on are incredibly important things.
A simple version of what we [at Flagship Pioneering] do for a living, in a nutshell, is take the fiction out of science fiction. So, we all were brought up thinking science fiction is this esoteric area of literature that was frowned upon. There are no Nobel Prizes that I know of for science fiction; it is not valued. And yet in science, a lot of initial ideas and imaginary things start as science fiction. A subset of them over time remarkably become real.
“Imagine the world of possibilities and territories uncharted because it is not permissible to society.”
So, what faculty do we need to actually be able to do this? The answer is imagination. What do we do in our schools with imagination? We crush it. The more advanced education we get, the more we are supposed to be reasonable, knowledge-based and armed with nothing but the facts. But that is not where novel thinking comes from.
So, how do you express your imagination without looking silly? If I say something in front of you that is silly, you are going to think poorly of me. And yet, if I say something that seems crazy and then it becomes true, imagine the world of possibilities and territories uncharted because it is not permissible to society.
How does your team put this into practice at Flagship Pioneering?
Flagship Pioneering is a company that makes breakthrough innovations and forms companies that can then develop them into, hopefully, transformative products. We’ve been around for 22 years. Currently, there are about 42 companies, mostly in the biotechnology therapeutic space, but also in agriculture and nutritional science.
Our specialization, if there is such a thing, is that we work on things that are normally impossible when we start. They are completely disconnected scientifically from the current reality. What we are doing is actually trying to prosecute the present for the future. So, we basically envision what could be possible.
Moderna, for example, was the result of such an exploration where we asked, could the body make its own drugs? And if you ask that question in that way, there is no academic work suggesting that the body could make its own drugs. There is work on RNA and DNA, etc. But if you ask the question that way—backward from the future— the present looks really different, and you go find bits and pieces in the present that you can combine to actually make something that does that. We do this process some 10 times a year.
All of Flagship’s companies come from our same scientific labs. Every company has gone through the same process. It starts with several “what if questions” followed by “turns out answers” that come out of our first dry experiments and then eventually wet experiments to practice. And then eventually we start building platforms that then generate pipelines that then generate products. That same methodology is underneath every single one of these companies we have created.
We keep our companies within the Flagship ecosystem and our ecosystem shares everything—meaning it shares the foundational IP when needed, shares expertise, regulatory insights, and how you manufacture capital. So, every dollar that comes into any of our companies is actually a source of capital for all the other companies. It is all one central ecosystem.
You’ve applied this imaginative philosophy to launch dozens of successful biotech companies over the past two decades. Now, how has the COVID-19 pandemic transformed and informed your approach to biotech innovation?
The biggest thing relating to the pandemic is the reconsideration of where in the spectrum of health to death we want to intervene. I would argue that right now, our system is geared to the 97th percentile toward post-disease. But is it really the case that you are well until the doctor tells you that you are sick? In between, what has happened to you?
The answer is you are in a state that we should in society openly call a pre-disease. Relating to the pandemic, if you get COVID, you have pre-disease. Keeping you in the pre-disease state should be our mindset. So, it is basically you are standing, you are falling, you have fallen. If the disease is “you have fallen,” it is really different because the damage is occurring when you are falling. If as you are falling, I can straighten you up, then what is that? It is preventing the actual fall or the disease. To do this, I have to act when we are in the process of getting data fast. To me, disease is an end state even though it may take a long time.
What if we train our algorithms, our measurement techniques, our interventions to focus on pre-cancer, pre-diabetes, pre-Alzheimer’s, pre-any number of things? Now, if I don’t have the disease, but still, I want to intervene, how do I do that today? I cannot because there is no way of working on it legally.
We need to think about pre-disease as a kind of a premedical condition. Doctors have to realize that you do not have to come to them only when you are sick.
“We need to demand the human right of getting actual health care, not sick care.”
Ten years from now, we should be talking about a category in between that is scientifically valid and that can be used to preempt, delay, derail and defer disease. That would be a great area of science.
But this mentality is entirely missing in medicine. Why? Because we focus on people who are close to dying and present with late-stage disease; they don’t present with early-stage disease, let alone pre-disease. Because those people occupy all our attention and all our empathy and all our money, we do nothing in early disease, let alone pre-disease.
So, you might say, why don’t health care providers consider whatever they can detect early disease? The problem with that is a practical one and not the way our regulatory and reimbursement system works in the United States. It is no disease, no reimbursement. No disease, no drug. You cannot test any agent that would be preventing falling at all. First, you have to let the thing fall. And then you have to show that this thing is going to improve once you’ve fallen. It’s crazy.
So, in the space that is upstream of disease today, there are supplements, and you know, “get well things,” but unfortunately, it’s largely pseudoscience. And the reason is that people do not have a mechanism to apply rigorous clinical science because the FDA will not let you. You cannot give patients molecules outside of an Investigational New Drug application.
Well, that’s nuts, because there are a lot of molecules we ingest today, mainly in food, and there are a lot of drugs we have taken that are in the general Pharmacopeia, which have safety data in humans. And they should at least comprise a starting point from which we can actually work on this.
So, we are trying to come up with ways to intervene with pre-diseases, not treat diseases, to keep pre-patients, not patients, on as long a journey as we can before they become patients. It sounds reasonable but is completely unreasonable within the current order of things.
Often, after epidemics or pandemics resolve, organizations and society experience a sort of “pandemic amnesia.” Has the pandemic been so monumental that these lessons learned will carry forward, or might things return to business as usual? What lessons do you think will endure?
This is a wake-up call. We need to demand more and not relent. I think that we need to demand the human right of getting actual health care, not sick care. And that demand would cause a re-evaluation of the entire system.
I cannot wait until this pandemic is over. Not for the reason you might think, but because I think it will begin an age of reckoning of what is broken and what we can do to fix it. My biggest fear is that the minute this pandemic is over, we will get on with some other things and completely lose the moment, not just for vaccine preparedness, but for all aspects of health care.
I will say personally, I lost my father-in-law to COVID-19 within a month of the disease starting in Sweden. I fear the notion that he or the other likely 20 million people that have died from COVID-19 have sacrificed their lives for the ones who survived to go back to living the same way. It is kind of like World War II. There was a long period of time where people had a reckoning and they said: What institutions do we need? What interventions must we have? What do we need to do to protect diplomacy? We need to consider all of these questions amid COVID-19. And if we do not, this is going to continue to be the age of disease.
Unfortunately, it is too early to see signs of us doing these things because it almost feels like we are still in the fight, and therefore, we are taking our attention away. So, what I am saying is there is going to be a bridging period where I hope people— whatever their passion is and whichever angle of a broken system they want to work on— will actually latch on for the sake of whoever they know who lost their lives.
I’ll add one more thing. Not to be the bearer of bad news, but you should find out what is happening day after day in publications on long-COVID. Long-COVID is a serious, serious issue. I know personally. My mother-in-law who got the disease at 90 years old and survived has had two major clotting events since. The chance of me having that experience and millions of other people is not very unlikely.
The effect this new disease is having on our health is quite unprecedented. We are going to have to study it carefully and intervene quickly if we are to counteract it. But if, as soon as the pandemic is over, we say well, it is not really a disease; it is a syndrome and we are not sure what to do about it and then it will dissipate. You are going to have tens of millions of people living with these conditions.
Based on your vast experience and unique insight into biomedicine, what health innovations or technologies are likely to be transformative over the next decade?
First off, the role of machine learning and AI in life science, not just in medicine, will be enormous because the human capacity to deal with the complexity of biological systems is trivial. In other words, there is no way we can deal with 10,000 proteins that are interacting in one hundred thousand different ways, let alone in one trillion. That is just completely untenable.
The notion that we are going to publish papers the way we used to when we did not know anything that was going on is crazy. AI, which I like to term augmented intelligence, will allow us to take bigger steps in our understanding.
Second, we have no idea how cells do what they do. Cells are kind of computational machines themselves. They have tens of thousands of parts, whether it is RNA or proteins that interplay to create the life of a living cell. As biologists, we think of them as their separate parts. We deconstruct the cell, look at all the parts and we have no idea how to reconstruct the cell out of the parts. Therefore, we cannot explain how it is that all of these moving parts do what they do—what we call reproduction or metabolism. With AI and machine learning, we are able to go after that. Instead of decomposing a cell, we can make measurements of an intact cell under very different conditions and begin to approximate what state changes mean and what drives them, so that we can begin to see cells in disease states.

Dr. Noubar Afeyan

Dr. Noubar Afeyan with Flagship Pioneering team members
We can then find ways to perturb the cells, regardless of where the target is. What you want is the cell to change its state through cell state change drugs, which have not been created so far. We have a company called Cellarity, and AI is enabling us to do a whole new generation of drug discovery that has never been done before.
A third one is by using some other technologies that have never been used in biology and measurement technologies in AI, we are finding that human cells make many tens of thousands more proteins than we ever knew possible. So, in our cells today, there’s the human genome and the human proteome, and we think we know all of the parts. But we are finding, through other measurement techniques, that there are literally tens of thousands of unknown proteins. We are the first, to our knowledge, to compare disease versus normal states and see many of these proteins elevated or reduced. Nobody has known to look. It is a little bit like astronomy, where if you look at one part, you see what you see and you think that is the universe. Then when you have a better high-resolution telescope, you see a whole bunch of other things and you say: Oh my God, I did not know those were there, but they may be weighing in on the things I am seeing.
Fourth, we are using machine learning and AI, through a company called Generate Biomedicines, to massively improve our ability to design de novo computationally designed proteins. By that, I mean we can take any sequence of DNA in a target protein and with no experiments, computationally create an antibody from scratch, because we have shown it millions and billions of different antibody sequences, and we have shown what causes this to bind to that. We can basically design an antibody, arbitrarily, to bind to any part of another protein. So, with computer-aided design (CAD), humans have designed airplanes and lots of things. We have never been able to design biologics. That computation has never been possible. Now, it has been about a 4.5-year-old effort. We have spent hundreds of millions of dollars developing it. And now we have created a computationally generated version of every protein that has ever been used as a therapeutic. The difference is our protein binds to the same place the drug does, so it can compute it except it is purely sequence-wise different. And there is no intellectual property on our proteins.
Lastly, the information molecule, which mRNA is, opens up a whole lot of other information molecules that I think we will be able to make drugs out of. So, one such molecule class is called tRNA—transfer RNA—which we have the only company that has been working for several years to convert into drugs. What tRNA does is it literally recognizes a triplet codon of DNA and in the mRNA stage, converts it into amino acids. So, mRNA is processed by a ribosome and tRNA is the decoder if you will—it is a molecule that bridges. So, if you can make a synthetic tRNA, it can correct a genetic code error in the protein that has that error and allow the correct protein to be made. It is not gene editing. We are not doing anything to the genome, but we are doing it during the processing and the translation of RNA to protein. So that technology is under development at a company called Alltrna. It is as far out from today as mRNA was 10 years ago from what had been done before.
The more we have learned about the basic molecular building blocks of life, the more we realize life is just information technology. And with that comes speed and determinism and we need to design a system to be able to handle that.
Those are just a few, I could give you a dozen more.
This interview has been edited for length and clarity.
Dr. Deepak Chopra and Dr. Robin Smith at the Dubai YPO evening event
If you have any questions or feedback, please contact: curalink@thecurafoundation.com
Newsletter created by health and science reporter, Ali Pattillo and associate director at the Cura Foundation, Svetlana Izrailova.