With World Brain Day occurring on July 22, it couldn’t be more timely to share a conversation with Dr. Sanjay Gupta, CNN Chief Medical Correspondent and associate professor of neurosurgery at Emory University Hospital. In his latest book, Keep Sharp, Dr. Gupta challenges conventional wisdom about neuroscience and outlines a powerful roadmap to optimizing cognitive function throughout life.
A conversation with Dr. Sanjay Gupta
Dr. Sanjay Gupta has been a trusted voice in media for over two decades, helping the public navigate perilous health crises, world wars, natural disasters and most recently, a global pandemic. In his recent book, Keep Sharp, Dr. Gupta turns his focus toward another fear-inducing threat: Alzheimer’s disease and dementia.
Drawing from his experience as a neurosurgeon, hundreds of interviews and extensive literature reviews, Dr. Gupta says the data is clear: Cognitive decline is not an inevitable part of aging. In fact, it’s possible to optimize brain health throughout life—a spectacular realization that should offer hope to many. As Dr. Gupta notes, the seeds of dementia are planted years before dysfunction appears, suggesting we have more power to keep our brains healthy than previously thought.
In Issue 5 of CuraLink, Dr. Gupta will change the way you think about your brain—and offer actions you can take today to build cognitive resilience for years to come.
Sanjay Gupta, MD, CNN Chief Medical Correspondent and associate professor of neurosurgery at Emory University Hospital
For decades, you’ve been a leading global voice on brain health as well as a practicing neurosurgeon and science communicator. Was there a moment or experience when you fell in love with the brain?
I don’t come from a medical family, so there wasn’t this pull when I was growing up to be a doctor. My parents are mathematicians and engineers so, as a child, I thought that is what I would become as well. But then in
my early teens, my maternal grandfather had a stroke. We were very close, and I visited him frequently in the hospital. This was the first time I spent a lot of time in a hospital and at the same time got a sense of the mysterious and surprising ways the brain works.
I remember that he had an episode where he could write but could not read what he wrote. That was a pivotal moment for me. I was a young teenager, but I was becoming fascinated with how the body functions. The brain just really spoke to me at that point—my desire grew to understand as much as I could about it. I can’t say at that time I knew that I would become a brain doctor or even a neurosurgeon, but it was then that I started to learn and talk more about the human brain.
As you trained as a doctor and a neurosurgeon, were there any experiences that transformed the way you thought about the brain?
When I started my neurosurgical training, I was amazed at how well the brain could recover from traumas, tumors and aneurysms or bleeds—situations where I was not very optimistic about a patient’s recovery, then slowly over time, they continued to improve. It gave me a sense of just how much regeneration and plasticity the brain really has.
When I was on call one night, a 93-year-old man came in with a bleed on top of his brain. It is called a subdural hematoma, and it is usually from trauma. I remember thinking: Is he in good enough shape to tolerate an operation? I spoke with the family, and they said he was in great shape. In fact, he had injured himself because he had been on the roof using a leaf blower, which gives you an idea of his physical capacity.
In the operating room, I looked at his brain after removing the blood collection. It looked like the brain of a 93-year-old—it was shrunken and had deep crevasses, which happens as you age. But its function was still extraordinary. Afterward, in the recovery room, he was already looking at his phone following elections in West Africa where he had volunteered with Habitat for Humanity a couple of years earlier. He was cognitively very functional and was still working as a stockbroker. We are entering an era where that can be the norm, rather than the exception.
We have these preconceived notions of this preordained decline or wear and tear that we associate with other parts of our body such as our joints and other organs.
“When it comes to the brain, it is spectacular to realize that it can actually grow sharper as you get older.”
In many places around the world, people have high cognitive function their entire lives. That was interesting to me. I have had a lot of conversations about it with my parents and others, asking: What is it that we expect of our brains?
What are the major research breakthroughs that have revolutionized neurology and neuroscience?
When it comes to the big disease “buckets” of the brain, it is split into three: tumor, trauma and bleeding (from aneurysms and the like). We continuously make breakthroughs through innovation such as improving diagnoses, using operating microscopes, improving
treatments with new therapies and enhancing screening and treatment for aneurysms. But those are still very much disease-oriented buckets. We have not made as many breakthroughs when it comes to truly preventing disease or even optimizing brain function.
For a long time, the brain has been considered this black box— something that was measured by its inputs and its outputs—but people did not have a clear understanding of its inner workings.

Dr. Sanjay Gupta and his surgical team operating in Port Au Prince, Haiti, following the devastating earthquake that hit the country on January 12, 2010
I was likening it the other day, with one of my daughters, to the docuseries “Night on Earth.” The low ambient light cameras they use are amazing allowing us to see animal behavior at night like we have never seen before. We assume these predatory hostile animals are that way all the time. At night, however, you see them lovingly playing with their cubs. Rare animals that you never get a sight of during the day are suddenly frolicking on riverbanks.
The point is that if we get a glimpse at the healthy brain, not just the diseased brain with a tumor, trauma or blood, we see something remarkable, which is that the brain continues to regenerate throughout its entire life. Previous conventional wisdom said you got what you got, you drain the cache over time, and that was it. But the brain does continue to regenerate and build new cells. That is significant.
There have been other big research breakthroughs in deep brain stimulation such as using small .35 millimeter probes to stimulate a certain area of the brain to treat addiction, obsessive-compulsive disorder, Tourette Syndrome and the like, which we have not had good therapies for. Now, potentially, through stimulation of the brain in these specific areas, we can change the brain. But we have not made as much progress in finding effective treatments for what worries most people, which is dementia.
What are the consequences of neurodegenerative diseases like Alzheimer’s and dementia? Why is there a need for more investment and a new approach to these diseases?
This is in part why I decided to write the book. First, there is a fear factor. If you ask people over the age of 55 about what worries them the most—losing memory and fears of dementia or Alzheimer’s (which accounts for about 60 to 80 percent of cases of dementia) are always at the top. There are emotional and financial costs along with this fear. The fact that we have not had a significant, effective therapeutic in 15 years is very concerning. A recently approved drug, aducanumab (Biogen), went through two trials not showing much benefit and then a third trial showing incremental benefit. And it costs about $35,000 a year.
We do not have great therapeutics or options for patients once diagnosed. About one in nine people aged 65 and older has Alzheimer’s, and that number is expected to double over the next few decades. This could become one of the most significant neurodegenerative diseases of our time.
We talk a lot about heart disease, cancer and stroke. But dementia has not received the same amount of attention, particularly because we could not visualize the brain in the way that we can now. There are emotional and financial costs and significant consequences in terms of fear of Alzheimer’s and dementia overall. The United
Dr. Sanjay Gupta’s latest book, Keep Sharp
States and other developed countries are worse off than other countries. And we are not entirely sure why. But it is clear that some of the wealthiest countries in the world are the most affected by this.
What do you hope people take away from Keep Sharp?
Throughout early medical history, we focused on the diagnosis of disease. Treatment was a pillar that came later. Prevention is something that came about over the last quarter-century. Now, this idea of optimizing the brain and the body is a relatively new construct.
What I wanted to get across in the book was that the latest data makes the case that we can grow new brain cells at any age. Anecdotally, we may have known that for some time, but now we can prove it. A lot of people talk about plasticity—harnessing other areas of the brain to fulfill a deficiency in another part. That is different from true neurogenesis—the growth of new brain cells. Now that we know that happens, the question is: How do you do it?
In societies without much Alzheimer’s dementia, they do not have a magic therapy nor are they using something that we do not have. It is almost assuredly lifestyle beginning from a very young age. Even for younger people who are not worrying about this now, what they do now could potentially stave off the disease. What are those habits and behaviors?
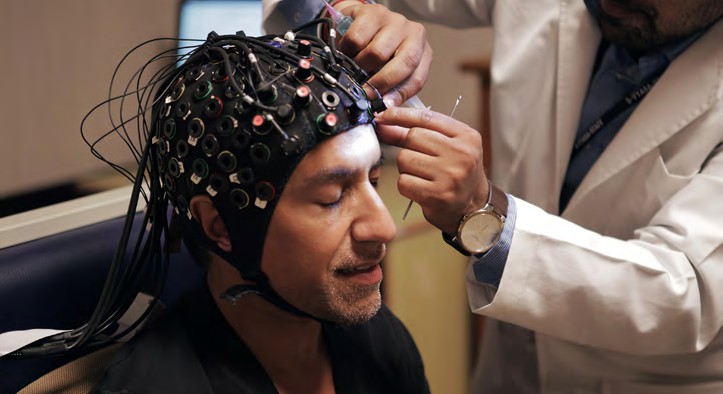
Dr. Sanjay Gupta undergoing neurological testing
So I followed some large control trials examining lifestyle changes and exploring the related benefits. How do you quantify that? One of the revelations for me was that we can now image the brain in ways that we could not before. Typically, people develop plaque in their brain decades before
they develop symptoms. If someone develops Alzheimer’s in their 60s or 70s, there is a good chance they had plaques in their brain in their 40s or 50s. But they were fine cognitively. So some people think: Well, that is frightening that I already had plaques. The other way of looking at that is that you had plaques and were still functionally fine. So it is not about removing the plaques, which is what so much of our therapy has focused on. It is about trying to build cognitive reserve and resilience. So even if you have the plaques, they are not changing how you cognitively function.
What role do early detection and novel diagnostic tools play in fighting dementia and Alzheimer’s disease compared to treating these diseases once symptoms appear or searching for a cure?
Certain biomarkers in the cerebral spinal fluid of someone who has mild cognitive impairment can now reveal with over 90 percent confidence whether or not that person is going to develop significant dementia in their lifetime. This almost becomes as much of an ethical as a medical question. If we do not have a really well-known therapeutic, do you want to know that this is going to happen? I would. There are ways you can plan your life. I have three kids, and there may be things that I would do differently for my family and myself if I knew that this was going to happen to me. Early detection also allows researchers to have larger clinical data about what really works. If we are only diagnosing people late, when their symptoms are advanced, it is harder to do meaningful studies. You want to catch this early, be able to do studies early and hopefully figure out prevention strategies. That is probably one of the biggest keys of early diagnostics.
All sorts of things we do regularly are probably accelerating our decline—uncontrolled or even slightly high blood pressure, exposure to pollution, not moving enough, not building cognitive resilience and redundancy. Early diagnosis tends to inspire people to focus on that. It gives you a chance to prioritize your health.
Why should people be hopeful that with certain lifestyle changes they can stay cognitively healthy later in life?
We tend to get myopic in how we view certain diseases. Cardiac disease, for example, is the biggest killer of men and women in the United States. People think if there is heart disease in my family, it is going to happen to me. What we have seen time and time again is that genes do play a role. We can even test for certain genes
that put you at higher risk. But for the most part, your nurture, as opposed to your nature, is far more important, including with dementia. It is sort of an 80/20 split, to put a number on it, in terms of the impact of nurture versus nature. So use it as an early warning sign if you have a family history, but do not think that it is definitively going to happen to you.
In the United States, what is happening with dementia, numbers-wise, is frightening. But there are still many places in the world where it is so uncommon that they will write up a single case of dementia because it is so unusual. Whereas, we have millions of people who get diagnosed. So what is it that these communities are doing?
“It is possible for human beings to live their entire lives without inevitable cognitive decline.”
Even in places that do not have any of the additional resources that we have. It is inspiring and very optimistic to recognize that, then to figure out those traits or behaviors and see what can be easily translated to our lifestyle and educate people on it. That is what I tell people who are fatalistic about this. The only caveat is that I do not want to suggest that people who develop this lived a terrible life, which caused their disease. Who knows? It is tough to say.
Based on what I have learned from talking to neuroscientists all over the world for this book, a focus going forward will be on determining what accelerated these cognitive declines, especially in wealthy countries, and figuring out how to address that and reverse them.
What is your ultimate hope for the field of neuroscience and neurology?
We have long believed that our brain is going to naturally decline, and it is one of the most frightening things to deal with, especially as you get older. I am in my early 50s now, and it is something that I think about all the time. My dad had cardiac bypass surgery when he was 47. I thought about that constantly, believing that it was preordained. But when I was in medical school, I realized that I could outrun my family history if I engaged in certain healthy behaviors. The same can be said for your brain.
We have not thought about the brain that way—as something that we could modify or improve in some way. We thought about it as immutable or fixed. For most people, young and old alike, as much as we want to improve our brains, we have not done anything to make that happen because we have not thought it was possible. That is the biggest lesson.
If you optimize your brain earlier in life, the data shows that you are much more likely to stave off dementia later in life. It took me close to three years to write this book, because I kept going back to these neuroscientists to make sure that we were stating things that A) were true, and B) were adaptable and useful in people’s lives. What I learned is that it is not that hard, but it is not totally easy either, and it should not be.
“We are dealing with the most enigmatic three and a half pounds of tissue in the known universe.”
We are dealing with a supercomputer that is thousands of times more sophisticated than any man-made computer. It should be hard, to some extent, to maintain brain health and ward off future problems. But it can be done. And it does not involve a new therapeutic or technology. It involves a lot of what we already know.
What are the most effective strategies people can use to prevent neurodegenerative disease and optimize cognitive function as they age?
When researching and writing Keep Sharp, I wanted to make sure I reviewed the best data behind what works. My North Star was the idea of neurogenesis, building new brain cells. We know it happens constantly in our brains.
We are all doing it right now. But some people are doing it much more efficiently, much more robustly, and it is not declining as they get older.
The aspect that has the most evidence behind it is movement. But conventional wisdom has always been that what is good for your heart is good for your brain. To some extent, that is true, but it is more nuanced. Movement, especially brisk movement, tends to lead to the release of BDNF or brain-derived neurotrophic factor. This is not something you can inject or take orally. Your body makes it, and as a famous neuroscientist described it to me, it is like Miracle-Gro for your brain. BDNF is the stuff that promotes neuronal propagation and growth.
Intense movement and vigorous exercise also cause BDNF release. But the problem is you are also releasing so much cortisol that it tends to mitigate the impact of BDNF. So intense exercise might be good for your heart but is not as good for your brain. Moderate activity and brisk walking may be better.

Dr. Sanjay Gupta and his family at the Taj Mahal
When it comes to diet, reducing sugar intake is crucial. We know that human beings eat a lot of sugar. In the past, we ate very little of it. When fruit fell from the trees, we got sugar, and bees protected even the honey. Now we are eating, on average, 130 pounds of sugar a year. We know that the body is very effective at internalizing that and turning it into stored energy, which usually is in the form of fat. That is what the body does—it is planning for a rainy day constantly. The brain does not work that way.
As soon as sugar levels go too high, glucose receptors in the brain do not keep taking in more energy but actually shut down. So you could be overfeeding your body and starving your brain at the same time, which is quite extraordinary.
That is why sugar is so problematic when it comes to your overall brain health. It is counterintuitive, but you are starving your brain of energy when you are eating a lot of calories. We may evolve into absorbing tons of energy into our brain, but right now we have a setpoint in terms of how much caloric energy we absorb.
When it comes to rest, and I use the word rest instead of sleep, what is fascinating to me is by imaging the brain, we see that there is a continuous sort of “rinse cycle.” In our body, our lymphatic system is constantly ushering away waste. Our brain has the glymphatic system to do the same. It is working all the time, but it is much more efficient when you are at rest. If you think about it, your brain is still active, but it is actively clearing your waste away, which may be the precursor for plaque formation. So make sure you get plenty of rest.
People focus a lot on brain training in the form of crossword puzzles, Sudoku, etc., which is great. But when it comes to your brain health, the data shows that doing those exercises makes you really good at doing those sorts of exercises. It is like driving the same road every day; you know how to get to work; you can do that with your eyes closed.
Doing other things that are totally different is the basis of building cognitive resilience or cognitive redundancy. So it is not about getting really good at doing one thing, although that can be great. If you are trying to build cognitive resilience or redundancy, doing different things is helpful.
For example, I’m a terrible artist, but I paint now. And to add even more redundancy, try doing things with your non-dominant hand. I paint with my left hand. If you can find activities to do, especially ones that involve motor strength or the motor cortex, something using your hands, that is even better. So those are some examples of how you move, how you eat, how you rest and the types of activities that make a difference.
Also, during the pandemic, we were not able to participate socially as much as we used to. I have never been a super social person, but I realized that I did miss it in ways that I had not anticipated.
I hate to make something that is so beautiful and social, clinical, but the idea is that you release oxytocin when you socialize, which is the feel-good hormone. Mothers release this when they have babies. It allows you to bond with people. We also see the relationship between oxytocin and BDNF. So being social while briskly walking is probably one of the best things you can do for your brain.
Lastly, be vulnerable. When you are vulnerable and you ask for help from people, it tends to create profound social connections. Humans have always been very interdependent on one another. And as we become increasingly siloed, less likely to ask for help, less social and less likely to move, we are starting to get a picture of why we are in the position that we are in now. And I have just given you a very simple thing to help counteract that: Go for a brisk walk with a close friend or family member and talk about your problems. Ask for help. That could be a good way to help stave off future brain diseases.
This interview has been edited for length and clarity.
If you have any questions or feedback, please contact: curalink@thecurafoundation.com
Newsletter created by health and science reporter and consulting producer for the Cura Foundation, Ali Pattillo, and associate director at the Cura Foundation, Svetlana Izrailova.