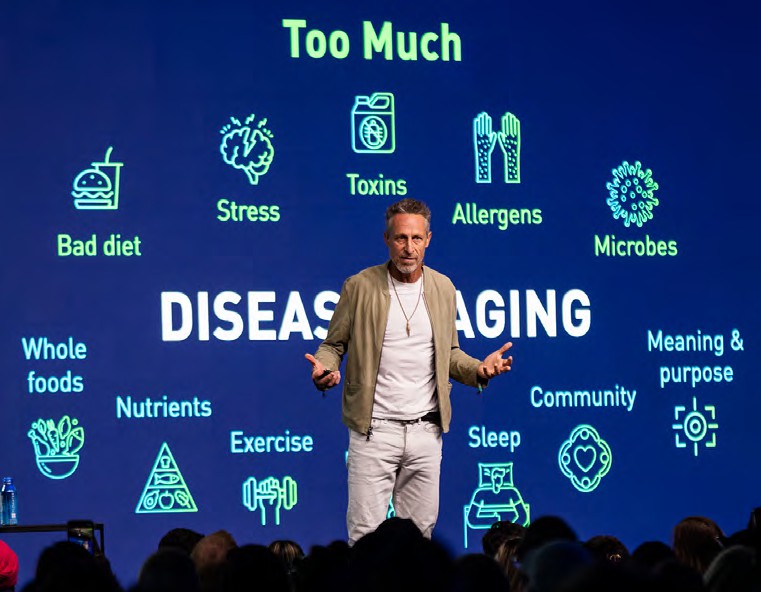
This month, we spoke with Dr. Mark Hyman, a physician helping lead a functional medicine movement to shatter health care’s status quo. Rooted in systems biology and holistic approaches, this field is more than a specialty; it’s a radical, yet intuitive, mode of thinking about and personalizing medicine. Dr. Hyman says it can revolutionize how we treat chronic disease and lead to optimal health.
A conversation with Dr. Mark Hyman
For Dr. Mark Hyman, functional medicine isn’t just a professional pursuit or clinical tool; it’s personal. After becoming sick with mercury poisoning in 1996, Dr. Hyman consulted doctor after doctor, but couldn’t find the answers or treatment he needed. It wasn’t until he was introduced to the principles of functional or systems medicine that he was able to resolve his symptoms and better treat those of his patients.
Since that recovery, Dr. Hyman has devoted his career to gathering evidence supporting this fundamentally different approach to traditional health care. A New York Times best-selling author and host of the leading health podcast, The Doctor’s Farmacy, Dr. Hyman has become one of the most recognized voices in integrative health care. He recently founded Function Health, an artificial intelligence, data-driven startup aiming to democratize health care through access to lab testing and the new paradigm of systems and functional medicine.
Functional medicine focuses on restoring physiological balance and harmony, not just symptom management. Armed with this approach, Dr. Hyman says we can better address the worldwide epidemic of chronic disease and help alleviate unsustainable healthcare costs.
What inspired you to pursue medicine and specialize in family medicine?

Mark Hyman, MD, fifteen-time New York Times best-selling author; Founder and Director, The UltraWellness Center; Founder & Senior Advisor, Cleveland Clinic Center for Functional Medicine; Co-founder and Chief Medical Officer, Function Health; Board President for Clinical Affairs, The Institute for Functional Medicine
In the early 1980s, I was studying Buddhism, a bit of systems theory and Chinese medicine at Cornell. My roommate was a PhD student studying nutrition and believed in the connection between food and health. We planted a garden and cooked fresh food for our meals. He also introduced me to nutritional scientists like Dr. Roger J. Williams who wrote Nutrition Against Disease.
I decided to become a doctor because I always felt drawn to helping people. After medical school, I worked as a rural family doctor for four years, then as an ER physician and eventually as a functional medicine practitioner at Canyon Ranch. Finally, I started my own functional medicine practice and began writing books to share the revolution happening in medicine. The rest is history.
Was there a turning point when you realized that the “conventional” healthcare system wasn’t working optimally?
Even before I became a doctor, I understood the challenges of our healthcare system from reading books like Ivan Illich’s Medical Nemesis and Kenneth R. Pelletier’s Mind as Healer, Mind as Slayer. I went to medical school with the mindset of a “subversive.” I decided to ingest and master the dogma so that I could move medicine forward to the next iteration I imagined was possible.
During your training, did you see these issues play out?
100%. The main tools in medicine today are pharmacological or surgical. Surgery can be very useful, but most chronic diseases don’t respond well to medication. It’s marginally effective at best or not effective at all.
Over time, it became clear to me that the system wasn’t helping patients. It was just managing their chronic illnesses, relatively poorly. Every illness I would see in my office had a cause. It wasn’t a lack of medication—a Lipitor® or Prozac® deficiency. There was something else going on. We needed to deal with the root cause.
When did you learn about functional medicine?
I was aware of integrative medicine early on through Dr. Andrew Weil and Dr. Deepak Chopra. Then, about six months after I started working at Canyon Ranch, I became very ill with what would be later diagnosed as mercury
poisoning. I had severe chronic fatigue syndrome, digestive problems and immune issues. I was a mess. I went to doctor after doctor. Nothing was showing up in my tests, but I knew it was real.
One of my colleagues invited me to a seminar with Dr. Jeffrey Bland (who is frequently referred to as the “father of functional medicine”). I went and thought: “Either this guy’s crazy or he is a genius, and I owe it to myself and my patients to find out if what he was saying was true.”
I became an intellectual vacuum cleaner and sucked up every bit of information I could about functional medicine. I used it on myself and on my patients. The results were remarkable. I started to get better, and so did they. I thought: “Wow, this is something real. I wanted everyone to have access to it.”
How do you define functional medicine, and what sets it apart from other modalities?
Functional medicine is essentially a description of the laws of biology, as opposed to a reductionist disease- based model. It’s agnostic when it comes to therapy or treatment. So, in other words, if the treatment is surgery, we do surgery; if the treatment is a drug, we prescribe a drug. I wouldn’t call it alternative medicine. Alternative medicine involves things like acupuncture, Ayurveda, homeopathy and Reiki, which can be useful. Integrative medicine means incorporating those alternative therapies into traditional medicine. It may prescribe meditation along with taking your blood pressure medication or suggest getting acupuncture with your arthritis medication.
The difference with functional medicine is that it’s a systems biology approach to health and health care. Integrative medicine involves some of the tools, but functional medicine provides the map.
“Functional medicine is the science of creating health, as opposed to the science of treating disease.”
The philosophy is similar to traditional ancient systems like Ayurveda or Chinese medicine, which focus on restoring balance and health. The same goes with functional medicine; it’s about restoring health and as a side effect, disease goes away. I don’t treat diabetes with medication. But if I provide healthy conditions via nutrition, exercise or supplements, the diabetes goes away.

Dr. Mark Hyman is one of the most recognized voices in functional medicine. He is a New York Times best- selling author and host of the leading health podcast, The Doctor’s Farmacy
Functional medicine takes an ecosystem approach. It’s really understanding the body as a network of networks. Systems medicine, network medicine and functional medicine are different names for the same approach. Our biology is not as we describe it in medicine today, which is based on a reductionist model and a phenomenological description of symptoms or signs.
For example, if someone’s sad, hopeless, helpless, has no interest in social activities or appetite and can’t sleep, people think that depression is the cause of their symptoms. Well, it’s not the cause; it’s the name of the symptoms. The cause of their depression could be gluten sensitivity, vitamin D deficiency, omega-3 deficiency, ingesting too much mercury, type 2 diabetes or a million other things. In functional medicine, we ask: “What’s out of balance, and how do we restore balance?”
From your perspective, what are the major shortcomings of our current healthcare system that a functional medicine approach helps fix?
There are two key problems: One is the overall paradigm and the second is reimbursement.
First, medical schools are still teaching as if it were the 1920s. The training is based on an anachronistic idea that there’s a single vector that causes a single disease with a single drug treatment. In other words, for instance, pneumococcal bacteria cause pneumococcal pneumonia and can be treated by penicillin. We’ve charged down that path, which works for some conditions like certain infections or vitamin deficiencies. But it’s not always accurate.
Look at COVID-19. Why did the U.S. make up 16% of the world’s deaths, when we’re only 4% of the world’s population? Because most Americans are pre-inflamed, chronically ill and overweight, all of which make us susceptible to hospitalization and death due to COVID-19.
The current system is focused on symptoms and diseases not mechanisms and causes. Functional medicine fundamentally changes that. It also incorporates an understanding of network biology, which is currently completely absent from conventional training and practice.
I’ll give you an example. I treated a female patient in her early 50s at the Cleveland Clinic. She had severe psoriatic arthritis with joint pain, inflammation and skin rashes. She was pre-diabetic and overweight and had acid reflux and irritable bowel syndrome (IBS). She also had migraines and depression for which she took Prozac.
She was seeing various specialists and was on a different drug treatment for each symptom. These were the best-in-class treatments from the best doctors at the Cleveland Clinic, which is one of the top healthcare systems in the world. But she wasn’t getting better. She was barely managing day-to-day and her medication bill was probably about $60,000-70,000 a year.
I thought: “How are all of these symptoms related? Inflammation. Where does inflammation come from? Usually the gut.”
It turned out that she had small intestinal bacterial and fungal overgrowth, food sensitivities and many nutritional deficiencies. I prescribed an elimination diet: a whole-food, anti-inflammatory diet without gluten, dairy, sugar or processed food. I gave her an antibiotic to kill off the bad bugs in her gut and an antifungal to kill off the yeast.
Then I repopulated her gut with healthy bacteria and gave her some basic vitamins. Six weeks later she came back, and everything was gone. Psoriasis, arthritis, headaches, depression, reflux and IBS all resolved. She lost 20 pounds and was no longer pre-diabetic. I wasn’t treating any of those diseases. I was just restoring her gut ecosystem and removing inflammation triggers. Then her body knew what to do.
You don’t get that result using the dominant medical approach.
“The whole gamut of diseases that is bankrupting our country and causing massive amounts of suffering is needless.”
It’s not that we have bad doctors or a bad medical system. It’s that we are applying the wrong tools to the problems we are facing. We have a thinking problem.
The second problem is reimbursement. Our entire system of education, reimbursement and practice is based on this old paradigm. We don’t get paid to do what actually works. We get paid to do what will be reimbursed. Well- designed integrated lifestyle and nutrition change programs work. But they aren’t paid for. So, we don’t do them.
Does functional medicine outperform the standard of care?
Yes, it does, but there’s a lack of adequate research on it. Forget about functional medicine, there’s little funding for nutrition research despite poor diet being the major cause of death and illness worldwide and the biggest contributor to our exorbitant healthcare costs.
In 2021, my colleagues and I published a study that had been conducted at the Cleveland Clinic showing that when compared to a matched cohort
in a traditional family practice, a functional medicine approach did better across every metric. Another study published in 2020 looked at autoimmune disease. The rheumatology department did the analysis and could have been potentially biased toward conventional treatment in reporting the data, but they found that our practitioners were better
in validated metrics for outcomes for rheumatoid arthritis and psoriatic arthritis.
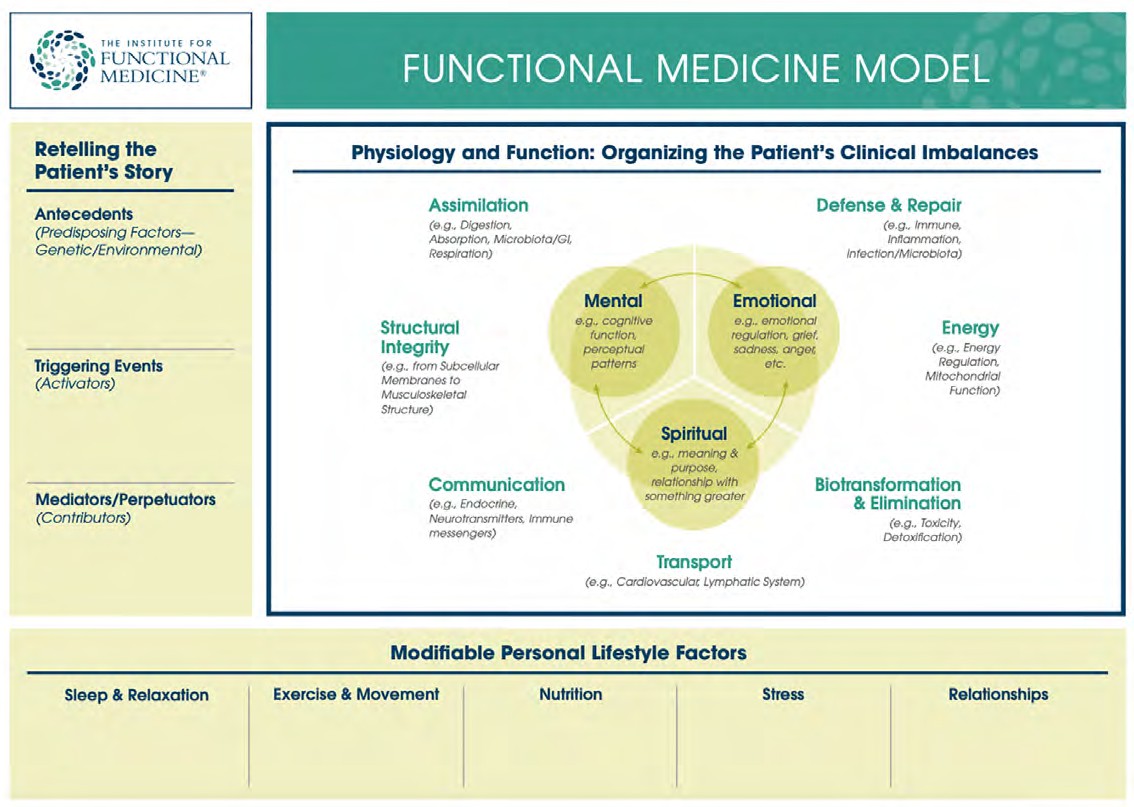
The Functional Medicine Matrix. Functional Medicine helps clinicians identify and ameliorate dysfunctions in the physiology and biochemistry of the human body to improve patient health. The most important rule of this approach is that restoring balance—in the patient’s environmental inputs and the body’s fundamental physiological processes—is the key to restoring health (The Institute for Functional Medicine, 2015)
So, there is good emerging evidence of better outcomes, but that’s not enough. The problem is: If you’re studying an arthritis drug, you randomize the drug among a group of people. It’s one drug, one disease. But complex illness is multi-causal and requires multimodal therapies. It’s like saying: “To study longevity, we’re just going to experiment with food and exclude exercise, sleep and stress.” You have to deal with all of it. But it’s hard to do research like that, and it doesn’t get funded.
That said, there’s a lot of evidence on nutrition, the microbiome and lifestyle that is in the functional medicine realm. It works well for pretty much every chronic disease that’s not acute or does not require surgery.
For the most part, it seems like functional medicine remains a luxury. What progress has been made to integrate it into standard care and get better reimbursement? What do you think it will take for this approach to be accepted?
At the Cleveland Clinic, we’ve developed an insurance-based model. Unfortunately, conventional medicine is not reimbursed for creating better outcomes or reducing costs. We get reimbursed for doing more procedures, more care, not for making people better. This results in misaligned incentives.
For example, that female patient who was able to get off $60,000 of medication benefited the insurance company. But the healthcare system and the providers didn’t benefit from improving her health. In fact, the healthcare system (other than the insurance company) will lose money because she is well.
I have a nonprofit called The Food Fix Campaign that’s focused on changing food policy. Right now, we have several bills for medically tailored meals and programs for nutrition services across Medicare and Medicaid. We’re also working on large-scale food systems change through regenerative agriculture.
It’s going to take a while for this to change, which is why I co-founded Function Health. We want to democratize access to data and provide insights and guidance based on functional medicine through data-driven machine learning-delivered decision support tools that help people improve and optimize their health. One of our other goals is research. We’ve already tested about 20,000 people, and we have over one million data points. Over time, as people follow the guidance and we track their results, we can publish more research.
How can consumers and patients distinguish between evidence-based functional medicine versus bunk or harmful practices?
This question is tough to answer because there’s so much misinformation. You need to do your own investigation. You must find experienced experts who have looked at the literature. It’s not that there’s no evidence. It’s that often doctors are not aware of it.
However, the evidence-based mantra is often a smokescreen that obfuscates a lot of things that work because it is held up as a holy grail. If something is not subject to a randomized, double-blind, controlled trial including over 10,000 people, then it doesn’t count. However, the majority of current medical practices have not been subjected to randomized, controlled trials.
It’s important for people to understand that research can be biased, funded by industry and massaged to create certain outcomes that may not be represented in the body of the paper—just written in the abstract or the conclusion.
“Everybody needs to be empowered to be in charge of their health and not abdicate that to the healthcare system or a doctor.”
Your doctor can be a partner, collaborator and expert to guide you. But at the end of the day, it’s your body.
What are the top three health practices that you recommend?
Doing an elimination diet is one of the best ways to identify how food impacts your health and to reset your biology. Everybody should try it for 10 to 14 days. I wrote a book called The Blood Sugar Solution 10-Day Detox Diet, which outlines how to remove unhealthy foods and add healthy foods. When you do that, many people’s problems improve or go away. It can even reverse diseases like type 2 diabetes. That is something I would highly recommend for people to determine how food impacts their health and their diseases. If you feel the same afterward, then great. But if everything you’re struggling with goes away, that’s a far more important piece of data than what you’re reading in a clinical trial. It’s your own body telling you what to do.
The second thing would be to understand that massive micronutrient deficiencies can play a role in our health. I’d suggest everyone take a multivitamin, fish oil, vitamin D and probably magnesium.
The third thing, aside from obvious lifestyle changes like exercise and diet, is to focus on gut health. You should incorporate prebiotics and probiotics as well as polyphenols in your diet through foods and potentially supplements. Do a deep dive on how your gut works and how to repair it.
Do you worry that patient pushback against the “conventional” healthcare system ever goes too far?
I definitely worry about that. Functional medicine is not anti-pharma, anti-surgery or anti-anything.
“Functional medicine is not anti-science. It’s actually the opposite.”
It’s finding the best approach for a particular person based on a personalized assessment. But there are people who see things in black and white. I had a patient with curable colon cancer. But she didn’t want to have surgery, chemotherapy or radiation. She wanted to heal naturally. I couldn’t convince her otherwise. And she died. It was heartbreaking. She left a husband and two kids.
If someone wants to access functional medicine, where can they start? How can people find a great functional provider, and are there enough providers out there?
Dr. Hyman sees a shift happening in medicine that mirrors what has happened in functional medicine for decades. According to Dr. Hyman functional medicine could help better address the worldwide epidemic of chronic disease and alleviate unsustainable healthcare costs
No, there aren’t enough, which is why I created Function Health to allow access for millions of people. There is huge demand but little supply.
In terms of finding a good functional medicine doctor, people can visit the website of The Institute for Functional Medicine. Try to find a certified practitioner with years of experience. It’s important to do your due diligence because the field is uneven. Also, ask around and seek recommendations from trusted doctors or friends.
What is your ultimate vision for an optimized functional healthcare system? Do you expect to see that in your lifetime?
I do think it will happen in my lifetime. Two things will change.
The economics are so bad that private employers, insurers and the government are realizing that the system can’t proceed with business as usual. Right now, there are many bills in Congress to try to address this—to mandate nutrition education in graduate medical education, for example. There’s a shift happening, which is good.
Secondly, most industries don’t get disrupted from the inside but from the outside. There are a lot of people trying to use tech to solve healthcare problems. But it’s like rearranging the deck chairs of the Titanic. The boat is still sinking, so it won’t matter. That’s where Function Health is different. We need a technology-enabled, AI- informed healthcare platform that empowers people to use their health data and provides guidance based on the science of creating health, most of which can be achieved without a doctor. It also offers decision support for those who have more serious issues and need a doctor. It also helps educate and provide decision support for healthcare providers.
Function Health’s portal will integrate electronic medical records, wearable data and lab results, which you can share with your health providers. So, ultimately, a patient could say: “Here’s what AI said that I should do. What do you think?” Then the doctor can advise. It creates more of a partnership.
We’re seeing different fields move toward this paradigm of network systems biology. For example, the science of longevity is mapping the hallmarks of aging such as inflammation, changes in the microbiome and mitochondrial dysfunction that are now understood to be fundamental processes that lead to all diseases of aging. We’ve been talking about these things in functional medicine for decades.
Anyone dubious about functional medicine just needs to ask: “How does the microbiome contribute to almost every known chronic illness including depression, heart disease, cancer, diabetes, obesity, dementia, autoimmune disease, allergies, asthma, chronic fatigue and fibromyalgia?” If you can’t explain how that works, you need to create a different paradigm to explain it.
If this is true, what do we do about it? How do we change medicine?
This interview has been edited for length and clarity.
If you have any questions or feedback, please contact: curalink@thecurafoundation.com
Newsletter created by health and science reporter and consulting producer for the Cura Foundation, Ali Pattillo, consulting editor, Catherine Tone and associate director at the Cura Foundation, Svetlana Izrailova.